Between 2009 and 2012 I completed a course in Chiropractic Paediatrics. This was the first time I learned about tongue tie. Like many of the other diagnostic tests and treatment protocols I was learning, I keenly went back into practice after that module to ‘save all the babies’ from tied tongues. I quickly found I had no one to refer to. So I would suggest to these mothers who were desperate to find a reason for their baby’s poor latch or persistent plagiocephaly (flat head) that a tongue tie might be the cause. Naively (on their part and mine!) they would head off to the paediatrician, only to be told there’s no such thing and that couldn’t possibly be causing the issue at hand. We would persist with the treatment I was giving, knowing in the back of my mind that there was definitely more we could be doing.
Fast forward a few years and two school friends’ babies were having food intolerance issues. I had been treating both their children, the thoughts of tongue tie and potential to correct or even get it assessed long gone in my mind. Hence, when tongue tie was diagnosed and corrected, then their symptoms improved, I firstly felt guilty I had let that knowledge go. But secondly, was excited that finally there were parents out there getting answers.
Part of my chiropractic training at university, my paediatric training and also the Applied Kinesiology courses I have attended have all had an element of Craniosacral therapy within the course. Craniosacral therapy involves very gentle palpation and mobilisation of the skull (cranio-) and pelvis, which includes the sacrum (-sacral). It is these parts of our anatomy, along with the spine, that house the entire central nervous system, our brain and spinal cord.
Many lactation consultants, dentists and other professional involved with the diagnosing and correction of tongue tie, advise ‘bodywork’ after the revision has been completed. Bodywork may be performed by a chiropractor, physiotherapist, osteopath or anyone else skilled in craniosacral or soft tissue therapy for babies. Finally I had somewhere to refer babies and in turn also started receiving referrals to do this bodywork.
When I became pregnant, I knew there was a high chance of my baby having ties. I was pretty sure my husband Josh was tied, my brother definitely is and we thought my Dad was too. When Harvey was born, it was really hard to look at him objectively. Also, when your newborn baby is crying, you want to be fixing that, usually with a boob, not looking in their mouth making diagnoses.
Feeding for us established fairly well. Harvey was born Tuesday and by Friday my milk had come in. That newborn period is a haze of feeding, napping, settling, changing nappies, staring disbelievingly at this baby that is finally here, more feeding, napping and settling, so the details are a little vague. But I think around two weeks was when feeding started getting painful.
My left side was far worse that the right. It actually started with a pain in my elbow. You know where you can hit your ‘funny bone’, well that’s your ulnar nerve. It sits in a little groove at your elbow and causes tingling and pain when you bang it. I had pain there, radiating up my arm. I remember constantly readjusting my position, thinking I might be leaning on that nerve. There’s so much going on at that time, it took me quite a few days to realise that pain was there every time Harvey fed. It worsened and spread up my arm and then the nipple pain and cracks started. The left side was cracked so badly, I thought the top of my nipple would just tear right off. Josh would bring Harvey to me when he was hungry and want to pop him straight on. I couldn’t do it. I had to mentally prepare myself every single feed. I knew it was going to be excruciating and it gave a real life example of toe-curling pain. I literally clenched my whole body while he latched and kept it tensed until he got into a rhythm. Even then it didn’t stop hurting, but it became bearable.
Harvey wasn’t suffering at all from what we could see. Except for when we had the fire too hot, making the house unbearably warm. He got a heat rash in his first week and we finally learned we were cooking the poor little thing. Apart from this, he was a happy, content, well-fed newborn. He had his moments, adjusting to life on the outside, but nothing out of the ordinary.
For Harvey’s birth, we had a private midwife, Marijke. We were very lucky that she was also a lactation consultant, well-versed in tongue ties. She knew from when he was born that there was an issue. At 19 days, Marijke assessed Harvey and concluded what she already knew, and I knew in the back of my mind, he was in fact tied. He had an upper lip tie and a posterior tongue tie.
An upper lip tie is when the piece of skin, called a frenulum, that attaches the lip to the gum right in the centre where the front two teeth will eventually be, is too tight. Everyone has a frenulum, but to be classified as a tie it needs to cause restriction. An upper lip tie stops the top lip from flanging up, allowing the baby to get a good seal when feeding. Without a good seal, they pop on and off causing nipple damage; they can swallow excessive air causing wind trouble; and the negative pressure required to draw the milk from the breast is lost. Also, this restriction doesn’t allow for the baby to open their mouth wide, which is essential for a deep latch.
Tongue tie is when there is a thick band underneath the tongue. There may also be a vertical membrane (piece of skin) present and the location of this restriction determines the classification. However, the level of classification is no indication of functional changes. Class 1 tongue tie is the most obviously to see. It causes a heart shaped tongue when baby tries to protrude it. This one is acknowledged by doctors and often dealt with. Class 4 is often missed (or denied of its existence). Class 4 means there is no membrane visible, but the restriction is further under the tongue, allowing the front and sides of the tongue to elevate, but not the posterior (back) portion of the tongue. Elevation of the posterior part of the tongue is extremely important in breastfeeding. That’s all I will say, as the mechanics of breastfeeding are too complex for this post. But it is also important in moulding of the hard palate (roof of the mouth) to ensure it is wide enough to accommodate all the teeth.
Dr Alison Hazelbaker is an International Board Certified Lactation Consultant. IBCLC – These are the letters you need to look for if you want somebody to assess your baby for ties. Dr Hazelbaker has developed the “Hazelbaker Assessment for Lingual Frenulum Function”. This was the assessment our midwife Marijke did when Harvey was 19 days old. He scored 10/14 for function and 4/10 for appearance. Anything less than 11 for function and 8 for appearance means that there is restriction. At this point, Harvey was still a happy and content baby. We had no issues with settling, fussiness, reflux, sleeping or wind. The only problem was my hesitation in feeding because of the pain. He did sometimes choke when feeding and we could tell there wasn’t a good latch as he was making clicking noises when he fed.
I received pressure from those around me to get him booked in immediately to have the ties released because in the past I had “no hesitation in sending other people’s babies off to get lasered” (in their words). My argument to that was that those babies had been brought to me by their mothers (or fathers) because they were experiencing symptoms (reflux, feeding issues, plagiocephaly, etc.) and at this point, Harvey’s ties were only affecting me.
After a few days of deliberation, we decided to book him in to get them reassessed and if necessary (which we knew it would be) lasered. Our reasons:
- He had started to get a bit of reflux. There is no way to tell if this would have continued or worsened but it negated my argument that it “wasn’t affecting him”.
- Josh had teeth removed and orthodontic work as a teenager (narrow palate) and we wanted to avoid that or minimise the risk.
- By the time speech issues are recognised, the child is already behind. Breastfeeding helps to develop tongue, mouth and jaw function ready for talking. If feeding is dysfunctional, this development may be too. While one can say, “We’ll wait until we see if there’s issues,” there’s developmental time already lost.
- If feeds are delayed, even subconsciously, this can affect milk supply. We didn’t want to reach four months and have my supply drop to a critical point. Supply can suffer or mastitis can occur if the breast isn’t drained properly, which can happen with dysfunctional feeding.
Within a week we had booked him into a dentist in Adelaide on his 6 week birth anniversary. Once the decision had been made and the appointment booked, I felt much better about the whole thing. I talked to Harvey about it. I told him what was going to happen, why we were doing it and that he would be much better off in the long run. Who was I reassuring? Him or me?
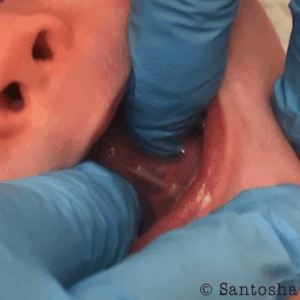
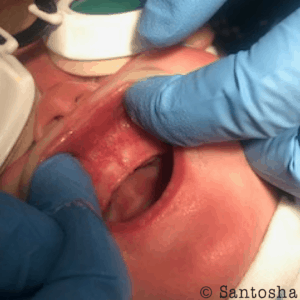
The most traumatic part of the whole experience was the assessment. He screamed as they filled his mouth with fingers, pulling this way and that, checking restriction, taking photos. Harvey was diagnosed with a Class 3 posterior tongue tie and a class 4 upper lip tie, with buccal (cheek) ties as well.
[one_half]
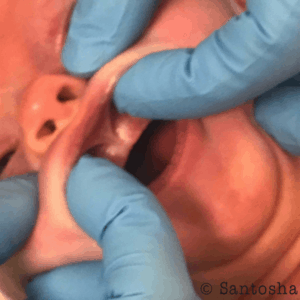
(Please do not use these images without permission. © Santosha Health & Wellbeing 2018)
[/one_half]
[one_half_last]
[/one_half_last]
We will be forever grateful to Marijke for making the trip down to our appointment with us because it meant that we could leave the room and Harvey still had someone in the room that was familiar to him. That was important to us. The nurse had said that it wouldn’t take long and if we stepped outside, she would come and get us. So we left our 6 week old, first born child, trusting them and walked outside. “Oh hey! Look, there’s coffee!” And we crossed the busy road to get a coffee. We obviously trusted them completely. We hadn’t even ordered a coffee when the nurse came outside looking for us. It was all done.
After the laser is complete, they help you do the first feed and make sure everyone is ok. Some Mums report that the feed is completely different, some feel that it’s the same. For me, it felt much the same. But he did seem to be opening his mouth a little more. Once they were happy and we were happy, we headed across the road for a debrief (coffee) with Marijke.
[one_half]
[/one_half]
[one_half_last]

[/one_half_last]
She explained that we were basically starting again. Everything that Harvey and I had learned about breastfeeding, we had to re-learn. All the neurological patterns that he had set up, he had to re-wire. She also prescribed Chlorsig Eye ointment for me to use in case there was a bacterial infection in the crack in the nipple that may stop it from healing.
It took a good four weeks for feeding to become easier. It was a gradual process where one day I suddenly thought to myself, “Yes, we’ve got this now.” During those four weeks, Harvey still dribbled milk and he still clicked a little bit but once the crack healed, there was no pain.
He’s nearly 5 months now and feeding is going great! When he wants to be, he’s super effeicent at draining the breast. When he wants to cuddle, he’s not efficient and lays there forever. About a month ago, he discovered his fingers and in the last few weeks his thumb. So now our battle is teaching him he can’t feed and suck his thumb at the same time. There’s just not enough room for it all in there!
I have absolutely no regrets or doubts about getting his ties lasered. It’s given me piece of mind regarding his palate for space for teeth and his speech development. It doesn’t mean he definitely won’t have issues in either department, but I know we’ve done what we can, as early as we could, to reduce his chances.
If you think your baby may have ties, I suggest you find an IBCLC in your area. There is also a Facebook group where many Mum’s post stories and questions. This group can be both helpful and overwhelming. https://www.facebook.com/groups/tiesupportaustralia but they have a list of preferred providers if you would like to see someone.
A non-exhaustive list of possible symptoms of tongue tie:
Babies
- Reflux or colic
- Clicking while feeding
- Shallow latch or slipping on and off the breast
- Wind pain
- Choking, gagging or spluttering
- Dribbling milk or drooling
- Falling asleep while feeding
- Uncoordinated sucking
- Poor weight gain or weight loss
Breastfeeding Mums
- Cracked, blistered or bleeding nipples (ouch!)
- Pain during feeing
- Misshapen nipples after feeding (flattened, creased, blanched or bruised)
- Mastitis or blocked ducts
- Low milk supply
- Vasospasm
- Thrush
- Exhaustion due to frequent feeding
Remember that this is not just relating to breastfed babies. Babies who are bottle fed with expressed milk or formula can also have issues. And it’s not just the short term that needs to be considered, but potential of long term consequences of altered tongue, jaw and dental biomechanics and function.

